Detailed content
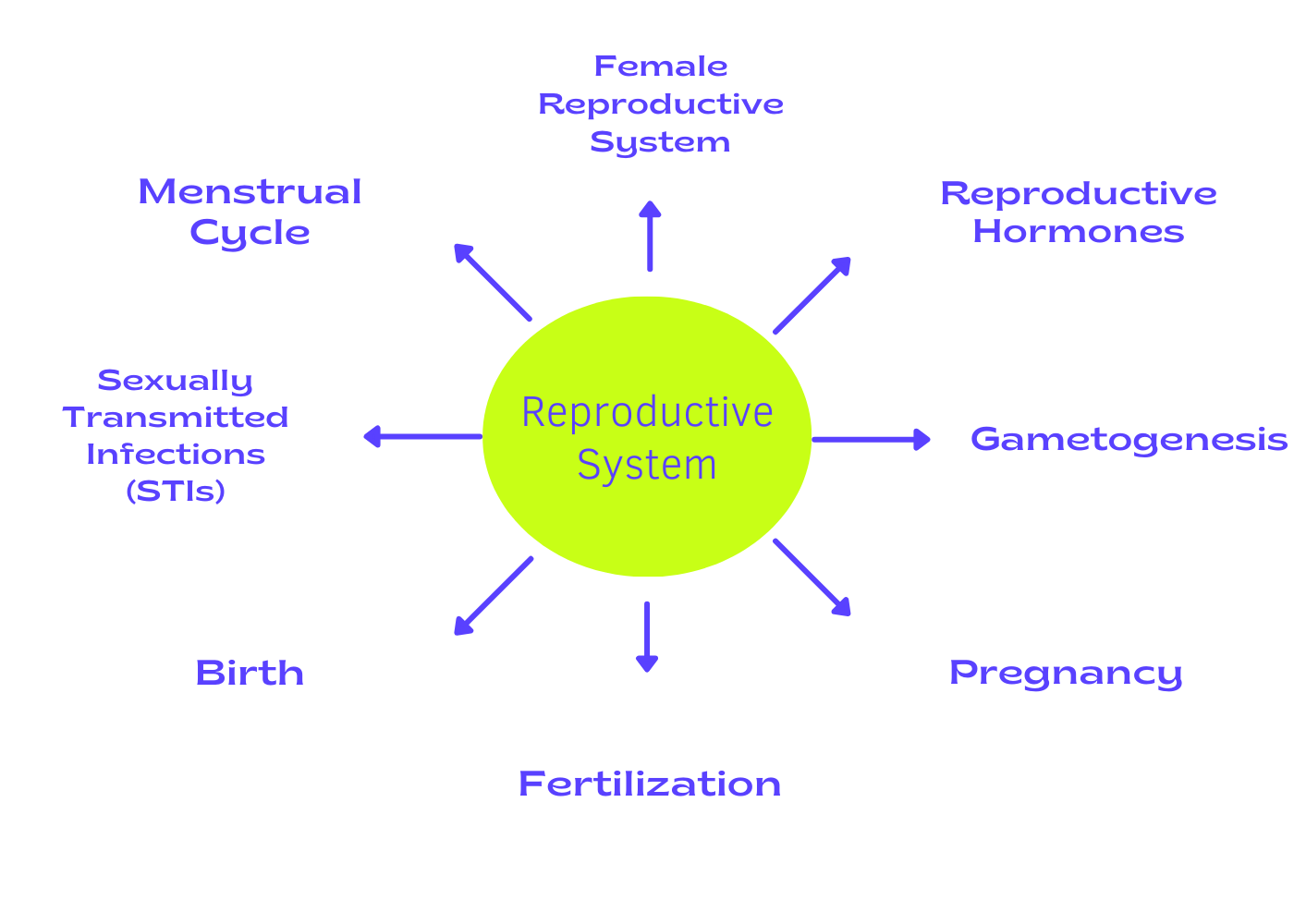
Introduction to the Reproductive System
The reproductive system is a complex network of organs and tissues
that work together to enable the process of reproduction. Its
primary function is to produce, nurture, and transport gametes
(sex cells) and, in females, to provide an environment for fetal
development. In males, the reproductive system produces sperm,
while in females, it produces eggs (ova) and provides a suitable
environment for fertilization, implantation, and fetal
development.
Anatomy of the Male Reproductive System
• Testes: These are the primary male reproductive organs
responsible for producing sperm and the hormone testosterone. The
testes are located outside the abdominal cavity within the
scrotum, which helps regulate the temperature necessary for sperm
production.
• Epididymis: A coiled tube located on the back of each
testicle where sperm mature and are stored before ejaculation.
• Vas Deferens: Also known as the ductus deferens, it is a
muscular tube that transports mature sperm from the epididymis to
the urethra during ejaculation.
• Seminal Vesicles: Glandular structures located behind the
bladder that produce seminal fluid, which nourishes and protects
sperm.
• Prostate Gland: A walnut-sized gland located beneath the
bladder that produces a milky fluid that mixes with sperm and
seminal fluid to form semen.
• Bulbourethral Glands: Also known as Cowper's glands, they
secrete a clear fluid that lubricates and neutralizes acidic urine
in the urethra prior to ejaculation.
• Penis: The male organ of copulation and urination,
composed of erectile tissue that becomes engorged with blood
during sexual arousal, resulting in an erection.
Physiology of the Male Reproductive System
• Spermatogenesis: The process of sperm production that
occurs within the seminiferous tubules of the testes.
Spermatogonia (stem cells) undergo mitosis to produce primary
spermatocytes, which then undergo meiosis to form haploid
spermatids. These spermatids mature into sperm cells through a
process called spermiogenesis.
• Hormonal Regulation: The hypothalamus releases
gonadotropin-releasing hormone (GnRH), which stimulates the
anterior pituitary gland to secrete follicle-stimulating hormone
(FSH) and luteinizing hormone (LH). FSH stimulates
spermatogenesis, while LH stimulates the interstitial cells of the
testes to produce testosterone, which is essential for sperm
production and the development of secondary sexual
characteristics.
• Ejaculation: During sexual arousal, the sympathetic
nervous system stimulates the contraction of smooth muscles within
the reproductive structures, leading to ejaculation. Semen, a
mixture of sperm and seminal fluid, is expelled from the urethra
through rhythmic contractions of the muscles surrounding the
reproductive ducts.
Anatomy of the Female Reproductive System
• Ovaries: The primary female reproductive organs that
produce eggs (ova) and the hormones estrogen and progesterone.
Ovaries are located on either side of the uterus within the pelvic
cavity.
• Fallopian Tubes: Also known as oviducts, these are
muscular tubes that extend from the ovaries to the uterus. They
serve as the site of fertilization, where sperm typically meet and
fertilize the egg.
• Uterus: A pear-shaped organ located between the bladder
and rectum that provides a nurturing environment for fetal
development. The inner lining of the uterus, called the
endometrium, thickens in preparation for implantation of a
fertilized egg.
• Cervix: The lower portion of the uterus that connects to
the vagina. It contains a narrow passageway called the cervical
canal, which allows menstrual flow from the uterus into the vagina
and serves as the passageway for sperm to enter the uterus.
• Vagina: A muscular tube that extends from the cervix to
the external genitalia. It serves as the birth canal during
childbirth and also receives the penis during sexual intercourse.
• External Genitalia: Also known as the vulva, these are
the external structures of the female reproductive system,
including the mons pubis, labia majora, labia minora, clitoris,
and vaginal opening.
Physiology of the Female Reproductive System
• Oogenesis: The process of egg production that begins
before birth and continues throughout a woman's reproductive
years. Oogonia (stem cells) undergo mitosis to produce primary
oocytes, which then undergo meiosis I to form secondary oocytes
and polar bodies. Meiosis II is only completed if fertilization
occurs.
• Menstrual Cycle: A monthly series of hormonal changes
that prepare the uterus for pregnancy. The menstrual cycle
consists of three phases: the follicular phase, ovulation, and the
luteal phase. During the follicular phase, FSH stimulates the
growth of ovarian follicles, each containing an immature egg. As
estrogen levels rise, it stimulates the thickening of the
endometrium. Ovulation occurs around the middle of the cycle when
a surge in LH causes the release of a mature egg from the ovary.
The luteal phase begins after ovulation when the ruptured follicle
transforms into the corpus luteum, which secretes progesterone to
maintain the uterine lining in preparation for implantation. If
fertilization does not occur, hormone levels decline, leading to
the shedding of the endometrium and the onset of menstruation.
• Fertilization and Implantation: Fertilization typically
occurs in the fallopian tubes when a sperm penetrates and fuses
with an egg, forming a zygote. The zygote undergoes several rounds
of cell division as it travels down the fallopian tube towards the
uterus. Once it reaches the uterus, the blastocyst implants into
the thickened endometrium, initiating pregnancy.
• Hormonal Regulation: The hypothalamus releases
gonadotropin-releasing hormone (GnRH), which stimulates the
anterior pituitary gland to secrete follicle-stimulating hormone
(FSH) and luteinizing hormone (LH). FSH stimulates the growth of
ovarian follicles and the production of estrogen by the ovaries.
Estrogen, in turn, inhibits the release of FSH and stimulates the
secretion of LH. LH triggers ovulation and promotes the formation
of the corpus luteum, which produces progesterone. Progesterone
maintains the uterine lining and prepares the body for pregnancy.
Reproductive System Disorders and Diseases
• Infertility: The inability to conceive after a year of
regular, unprotected intercourse. Causes of infertility may
include hormonal imbalances, structural abnormalities, genetic
factors, or lifestyle factors such as age, obesity, or substance
abuse.
• Sexually Transmitted Infections (STIs): Infections
transmitted through sexual contact, including chlamydia,
gonorrhea, syphilis, genital herpes, human papillomavirus (HPV),
and HIV/AIDS. These infections can cause infertility, pelvic
inflammatory disease (PID), ectopic pregnancy, or other
complications if left untreated.
• Endometriosis: A condition in which tissue similar to the
lining of the uterus grows outside the uterus, leading to pelvic
pain, infertility, and other symptoms.
• Polycystic Ovary Syndrome (PCOS): A hormonal disorder
characterized by enlarged ovaries with multiple cysts, irregular
menstrual periods, and symptoms such as hirsutism (excessive hair
growth), acne, and weight gain.
• Benign and Malignant Reproductive Tumors: Tumors or
growths that develop in the reproductive organs, including ovarian
cysts, uterine fibroids, cervical dysplasia, endometrial
hyperplasia, ovarian cancer, uterine cancer, and cervical cancer.
Reproductive System Disorders and Diseases
The human reproductive system is a marvel of biological
engineering, allowing for the perpetuation of the species through
the production of gametes and the nurturing of offspring. Its
intricate anatomy and physiology involve a complex interplay of
hormones, organs, and tissues, all finely tuned to facilitate the
processes of fertilization, gestation, and childbirth.
Understanding the structure and function of the reproductive
system is crucial for maintaining reproductive health and managing
conditions that may affect fertility and overall well-being.